

ACL Rehabilitation
Once an injury occurs, rehabilitation must take place to heal. Rehab can take weeks or months, depending on the severity of the injury. Many athletes do not take rehab exercises seriously and will not complete the rehab schedule. While many do the exercises, they do them incorrectly. One factor that causes many recurring injuries is poor technique during rehabilitative exercise. Many young athletes may never experience full recovery until they understand that improper technique is the cause of the ongoing problem. When you are in recovery, the information received can be beneficial and provide an analysis of recovery based on performance and personal commitment. This paper focuses on injuries to the Anterior Cruciate Ligament (ACL) and what it takes to overcome such adversity.
Cluett (2008b)[3] explained the function of the anterior cruciate ligament (ACL) as the primary resisting force to the forward motion of the tibia. The anatomical construction of the knee joint helps us understand this relationship (Cluett, 2008b)[3].
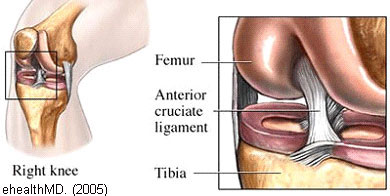
The femur (thigh bone) sits on top of the tibia (shin bone), and the knee joint allows movement at the junction of these bones. The joint would be unstable and prone to dislocation without ligaments to stabilise the knee. The ACL prevents the tibia from sliding too far forward. (Cluett, 2008b, p.1)[3] The ACL is a broad ligament joining the anterior tibial plateau to the posterior femoral intercondylar notch (Cross, 1998)[1].
The stabilization process of the ACL has four complex functions:
- It maintains mechanical stability.
- Restrains the anterior translation of the tibia.
- Prevents hyperextension of the knee.
- Acts as a secondary stabilizer to valgus stress by reinforcing the medial collateral ligament and controlling the tibia's rotation on the femur in femoral extensions of 0-30 degrees. (Cross, p.1).[1]
ACL injuries are common problems involving the knee joint
Recent studies indicate that 1 in 10 female college athletes has sustained this type of injury sometime during their athletic career. Research suggests that females participating in activities that "require cutting and jumping activities were five times more likely to suffer serious knee injuries compared to their male counterparts" (NWS, 2008, p.1)[7].
The ACL femoral attachment has a unique topography, with the lateral intercondylar ridge constant and often a bony ridge between the anterior-medial (AM) and posterior-lateral (PL) femoral attachment, known as the lateral bifurcate ridge. In the knee joint anatomy, an intercondylar notch lies between the lateral and medial condyles of the femur.
Some people are more vulnerable to the ACL than others, based on the osseous landmarks of its femoral attachment.
The ACL femoral attachment has a unique topography, with the lateral intercondylar ridge constant and often an osseous ridge between the anterior medial (AM) and posterior-lateral (PL) femoral attachment, commonly referred to as the lateral bifurcate ridge. In the knee joint anatomy, an intercondylar notch lies between the lateral and medial condyles of the femur.
The ACL moves within this notch, connecting the femur and the tibia, thus stabilising the knee. The ACL prevents the tibia from sliding forward and rotating medially. The majority of females have a small notch, therefore restricting ACL movement. "When movement is restricted, the femoral condyles can pinch the ACL within the joint, especially during twisting or hyper-extended movements, often resulting in a tear or rupture of the ligament" (Vlach, 2008)[11]. For some athletes, especially females, these attachment points may be smaller, contributing to female susceptibility to ACL injuries.
Assessment
An assessment must be done to determine what damage that has occurred with all knee injuries. "The knee needs to be examined systematically since so much can go wrong with the knee, and so many signs and symptoms may be produced, that only a systematic technique will ensure that nothing of importance is missed" (Neyret et al. 2008, p. 1)[5].
Three different tests can be performed:
- The Lachman test.
- The dynamic extension test.
- The Pivot Jerk test (Cross, 1998)[1].
M. Lemaire first described the most important of these three tests, the Pivot Jerk test, in 1968.
- The patient's foot is wedged between the body and the elbow of examiner.
- The examiner places one hand flat under the patient's tibia, pushing it forward (force applied in an anterior direction), with the knee in extension.
- The other hand is placed against the patient's thigh, pushing the other way (force applied in a posterior direction).
- The lower limb is taken into slight abduction by the examiner's elbow, with the examiner's body acting as a fulcrum to produce the valgus.
- The examiner maintains the anterior tibial translation and the valgus and imparts flexion. At 20°-30° flexion, pivot shifting will occur, with a clunk as the lateral tibial plateau suddenly reduces. (Neyret et al. p.14)[5].
 |
 |
When this procedure produces a shift rather than a clunk, the patient is unaware of the slip of the plateaus on the femoral condyles. The valgus component is less pronounced than the compression and anterior drawer applied by the examiner, producing joint play rather than a pivot shift, indicating a tear of the ACL.
Rehabilitation
Many variations of ACL rehab take considerable time to get back in proper physical condition. Each athlete has a specific rehab plan, even if many exercises are similar to another athlete. Each plan depends on a person's age, functional disability, and functional requirements (Cross, 1998)[1]. The significant goals of rehabilitation following ACL surgery are:
- Restoration of joint anatomy.
- Provision of static and dynamic stability.
- Maintenance of aerobic conditioning and psychological well-being.
- Early return to work and sport.
Following ACL reconstruction surgery, the range-of-motion exercises start immediately, with walking an essential component of post-operative rehabilitation. Being mobile during this time will help in achieving degrees involving the range of motion, with the initial focus on regaining full extension of the knee. In general, flexion (ability to bend) is much easier to gain than extension (Cluett, 2008a)[2].
A typical rehabilitation program consists of four distinct phases. During the first phase, the emphasis is placed on minimizing pain and swelling and maximizing motion. The main objective of the second rehab phase is to increase the range of motion. During stage two, the patient is subjected to resistance training designed to improve the range of movement through a well-designed regimen of lifting exercises specific to the quadriceps and hamstrings.
During the third phase, the goal is muscle control, increased strength, and greater endurance. At this stage, the range of motion should be completely restored. During the final rehabilitation phase, the subject will be encouraged to gradually work back into their sport (Palmer, 2005b)[9].
Working with physical therapists is one way to make rehab more successful. Therapists know what and where someone should be during their specific program. They can make sure that one is not overdoing it. Overdoing it could result in not healing the injury properly. Different exercises that one can do tolerably include heel slide, isometric contraction of quads, and prone knee flexion. Other exercises that can be done once able to stand include passive knee extension, heel raise, half squat, knee extension, and standing on one leg. (Quinn, 2006)[10]
Getting patients on a stationary bike is a good way to regain motion and improve strength. Other activities that one can do are working in a pool, on a trampoline, wobble board, and jogging, among many others. These activities are used during the different phases, so one should not be on a wobble board right after surgery. Take things slow and ensure that the injury heals so that one does not end up back at the beginning of rehab.
Once rehab is finished, the doctor will have the ultimate say in returning to a sport or working fully. The doctor's decision can be based on how well one did during rehab and the graft type (if one was done). Specific grafts are believed to take longer to heal, and therefore, the doctor may not want to push the knee too far too soon. The athlete may ask, "Should I wear a brace?" It all depends on the athlete. Some prefer a brace, while others do not. No studies show that a brace helps or harms one when wearing it (Cluett, 2008a)[2]
Palmer (2005a)[8] offers some encouraging information for all to consider: Many struggle to regain form after a serious sports injury and lengthy rehab period; some take months or fail. Returning to the form will be slow if we do not know what needs to be recovered. A natural talent for a sport comes from the right sort of conditioning. Good quality movement executed in the sporting activity creates appropriate learned movement patterns that reside subconsciously. (Palmer, 2005a, p. 2)[8]
Conclusion
Rehabilitation is defined in NRI (2008)[6] as a combination of methods focusing on restoring a subject's helpful life. Regardless of the disabling experience, rehabilitation helps the body achieve normal functions through different recovery techniques. Suppose a person has experienced a sports injury, an accident, or is incapacitated for other reasons. In that case, rehabilitation can improve movement functionality and help maximise personal health characteristics. Through rehabilitation, "not only are the physical aspects covered, but also the mental, psychological, and sociological aspects in achieving full recovery." (NRI, 2008, p. 1)[6]
Rehabilitation from injuries requires constant care by providing exercise therapies to regain muscles lost and recover from trauma experienced by allowing contact with other patients who have experienced similar injuries. Injuries involving young athletes' original skill patterns are often replaced by newly acquired, poor-quality action following a sports injury. Some athletes never regain the ability to realise their full potential after an injury requiring rehabilitation. (Palmer, 2005a)[8]
References
- CROSS, M.J. (1998). Anterior Cruciate Ligament Injuries: Treatment and Rehabilitation. Encyclopedia of Sports Medicine and Science
- CLUETT, J. (2008a). Rehabilitation After ACL Surgery. About.com: Orthopedics
- CLUETT, J. (2008b). ACL injury. About.com: Orthopedics
- ehealthMD. (2008). What is the anterior cruciate ligament? Health Information Publications
- NEYRET, P. et al. (2008). Examination of the knee joint
- NRI, (2008). Importance of rehabilitation. NewRehabilitationInfo.com
- NWS, (2008). Female ACL. New Wave Soccer Conditioning
- PALMER, R. (2005a). Rehabilitation: Time to Assess. Fitness Programs for Life
- PALMER, R. (2005b). Sports Injury Rehabilitation: Learn to take it Easy! Fitness Programs for Life
- QUINN, E. (2006). ACL Rehab Exercises. About.com: Sports Medicine
- VLACH, S. (2008). ACL and the female athlete: Theoretical causes and prevention. Life Fitness
Page Reference
If you quote information from this page in your work, then the reference for this page is:
- JACKSON, A. et al. (2009) ACL Rehabilitation [WWW] Available from: https://www.brianmac.co.uk/articles/article048.htm [Accessed
About the Authors
Lyn Ausdemore, Tyler Lathrop, & Zalie Limbach are all upper-division students seeking degrees with endorsements in human performance. Chris Green is a trainer for the athletic department, and Allen Jackson is an Assistant Professor in the Department of Health, Physical Education, and Recreation at Chadron State College.