

Patellar Tendinopathy
Patellar Tendinopathy is commonly known as "Jumper's Knee" and is caused by the Patellar Tendon overuse. This injury frequently affects athletes involved in jumping sports, which are included in a group of activities classified as high-impact sports. High-impact sports are physical activities that place above-normal force on joints, bones, tendons, and ligaments. These high-impact sports include basketball, dance, volleyball, soccer, football, track and field (distance running, high jump, and long jump), mountain climbing, figure skating, tennis, and skiing. Other people who may suffer from Patellar Tendinopathy include military recruits. This group is training in activities that strain the knee, making them more likely to develop Patellar Tendinopathy. The overall occurrence of Patellar Tendinopathy among sporting athletes has been estimated at 15%, with a higher prevalence of about 50% in elite jumping athletes, such as volleyball and basketball players.
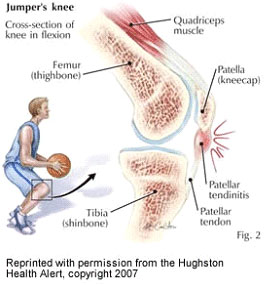 The critical warning sign of "Jumper's Knee" is a shooting pain just below the Patella, commonly known as the kneecap, when walking, working out, or performing daily activities. Overusing the Patellar Tendon represents approximately 15% of all soft-tissue injuries in athletes (Peers, 2005)[10]. When Patellar Tendon overuse occurs, inflammation of the Patellar Tendon gradually becomes more painful. In a survey independent of any treatment strategies, one-third of the athletes with Patellar Tendinopathy could not practice or participate in their sport for six months (Peers, 2005). Tendon overload occurs when "forces of 3 to 8% strain are applied to the tendon, which causes microtrauma", a minor injury to the connective tissue that may include micro-tearing of muscle fibres (Peers, 2005)[10].
The critical warning sign of "Jumper's Knee" is a shooting pain just below the Patella, commonly known as the kneecap, when walking, working out, or performing daily activities. Overusing the Patellar Tendon represents approximately 15% of all soft-tissue injuries in athletes (Peers, 2005)[10]. When Patellar Tendon overuse occurs, inflammation of the Patellar Tendon gradually becomes more painful. In a survey independent of any treatment strategies, one-third of the athletes with Patellar Tendinopathy could not practice or participate in their sport for six months (Peers, 2005). Tendon overload occurs when "forces of 3 to 8% strain are applied to the tendon, which causes microtrauma", a minor injury to the connective tissue that may include micro-tearing of muscle fibres (Peers, 2005)[10].
The forces applied when landing on the knee joint, Patellar Tendon, and other knee tendons may exceed nine times the participant's body weight (Donohue, 2008)[4]. There are various ways to avoid knee pain that involve strengthening the muscles surrounding the knee: the Gluteus Maximus, Quadriceps, and Hamstring muscles. Increasing the strength of the knee joint muscles will reduce the load placed on the knee joint. It also includes the forces on the Patellar Tendon. In addition to participating in strengthening activities, a conditioning plan that integrates common trunk and lower-limb stretching and plyometric training to increase endurance may assist in reducing excessive stress on the Patellar Tendon.
Risk factors contributing to the injury of the Patellar Tendon are inflexibility of the Quadriceps and Hamstring muscles, inappropriate overload of quantity and intensity of training, the hardness of the playing surface, and limited evidence of inherited biomechanical risk factors (Vulpiani, 2007)[11].
Findings Related to Patellar Tendinopathy
As stated previously, Patellar Tendinopathy, the overuse of the Patellar Tendon, occurs mainly in athletes who participate in jumping and high-impact sports. Patellar Tendinopathy may occur when rapid acceleration and deceleration, jumping, or landing from a jump. The affected sports cause inflammation in the knee joint, specifically in the Patellar Tendon. High-impact sports involve both feet leaving the ground simultaneously and other quick movements. Track and field events such as running or sprinting, tennis, skiing, soccer, and football are high-impact sports that pressure the knee joint and the Patellar Tendon.
In company with these common sports among athletes, another sport that affects the Patellar Tendon is greater in male athletes than in female athletes. This sport is dancing. Males experience more repetitive jumps in dancing than females (Mattingly, 2005)[9]. Patellar Tendinopathy may occur in males between the ages of fourteen and sixteen who experience a sudden growth spurt, characterised by the bones of the leg outgrowing the tendons and muscles of the leg. The unexpected athletes affected by Patellar Tendinopathy are military recruits during high-impact training.
The most common warning signs of knee inflammation are pain, aching, and swelling in the location of the Patellar Tendon. These symptoms may be found on the lower side of the patella on the front of the knee during walking, jumping, and exercising. Inflammation that occurs during Patellar Tendinopathy may be found in several areas. These areas include the top of the Patellar Tendon, the bottom of the kneecap, the bottom of the Patellar Tendon, and the top of the Tibia. The inflammation is caused by the overuse of the joint without a sufficient amount of rest (Donohue, 2008)[4].
The stages of inflammation are classified according to symptoms using a scale from zero to five, with five indicating the most pain. These stages may assist those suffering from Patellar Tendinopathy to determine the severity of the injury and the amount of activity that can be endured. Stage one is a minimal worry. The pain is only after activity, and all that is needed is rest. Stage two is a slight worry and pain before and after activity; rest may be needed. Stages one and two may respond well to a conservative intervention involving therapeutic exercise, ice, ultrasound, cross-friction massage, and rest (Klucinec, 2001)[7].
Stage three is more worry and pain during activity and less ability to perform satisfactorily. In stage three, prolonged rest and limited activity sessions are advised (Klucinec, 2001)[7]. Stage four includes increased worry, pain during activity, and inability to perform satisfactorily. In this stage, four further treatments may be advised. Stage five is very concerning pain during daily activity. In stage five, surgical procedures may be recommended. At Patellar Tendinopathy's worst, there will be pain while sitting or resting.
Classification of Jumper's Knee According to Symptoms
- Stage 0 - No pain
- Stage 1 - Pain only after intense sports activity; no undue functional impairment
- Stage 2 - Pain at the beginning and after sports activity; still able to perform at a satisfactory level
- Stage 3 - Pain during sports activity; increasing difficulty in performing at a satisfactory level
- Stage 4 - Pain during sports activity; unable to participate in sports at a satisfactory level
- Stage 5 - Pain during daily activity; unable to participate in sports at any level
Rehabilitation exercises are recommended to reduce knee pain caused by Patellar Tendinopathy. These exercises consist of strengthening, stretching, and plyometric training. Strengthening the Quadriceps, Hamstrings, and Gluteus Maximus muscles may reduce knee pain and the damaging effects of Patellar Tendinopathy. As the muscles above increase in strength, the tendon experiences less stress (Kongsgaard, 2007)[8]. The tendon will avoid being overused if its muscles have the strength to reduce the stress on the tendon.
Stretching the muscles around the tendon will increase flexibility in the joints to improve the range of motion and the ability of the joint to move smoothly through the movement. Stretching daily before and after workouts may reduce stiffness in the joints and remove lactic acid from the muscles. Plyometric training may improve muscle endurance. By improving the muscles' endurance, these muscles will endure increased stress for long periods without resorting to a tendon for more support, which may overload the tendon and cause injuries. Below are some tips on avoiding knee pain.
- Adequate warm-up before running or jumping (Dressendorfer, 1995)[5]
- Stretching program to maintain quadriceps and hamstring flexibility (Dressendorfer, 2007)[5] - Example: hamstring and quadriceps stretches (Delaney)[2]
- Strengthening techniques - Example: Half-squats and lunges can help strengthen (Delaney, 1995)[2]
- Correct any biomechanical errors in jumping technique (Dressendorfer, 2007)[5]
- Avoid repetitive jumping on a hard floor (Mattingly, 2005)[9].
Unavoidable risk factors that contribute to Patellar Tendinopathy are inflexibility of the Quadriceps and Hamstring muscles, the strength of the Gluteus Maximus, Hamstring, and Quadriceps muscles, inappropriate overload of quantity and intensity of training, the hardness of the playing surface, and limited evidence of inherited biomechanical risk factors (Vulpiani, 2007)[11].
Conclusion
Patellar Tendinopathy, commonly known as "Jumper's Knee," is the overuse of the Patellar Tendon. It is frequently found in athletes involved in jumping sports, such as volleyball, basketball, dance, figure skating, and many more. Any high-impact activities involving the lower body affect the "Jumper's Knee."
Examples of high-impact activities are sprinting, jumping jacks, and jumping rope. However, the full range of patients affected by Patellar Tendinopathy is not only found in sports. The pain of Patellar Tendinopathy may affect fourteen to sixteen-year-old males going through a growth spurt.
During basic training, it also affects military recruits participating in high-impact activities as part of their fitness preparation. Before symptoms relating to Patellar Tendinopathy occur, there are ways to prevent knee pain and injury. Knowing how to avoid knee pain may prevent the patient from sustaining an injury.
Common symptoms related to "Jumper's Knee" include pain, aching, and swelling on the lower side of the anterior surface of the Patella. Other symptoms include weakness and cramping of the knee joint. Common home remedies to treat "Jumper's Knee" include ice, rest, and anti-inflammatory medicine. Advil or Motrin may be used only in the early stages of injury.
If the injury symptoms are left untreated, the result may be knee surgery. A patient returning to physical activities should apply heat to the knee for 10 or 15 minutes before starting an activity. Following the activity, apply ice for 10 or 15 minutes (Dr Donohue, 2008)[4]. Conservative treatments heal and keep Patellar Tendinopathy at bay for more than 90% of cases (Vulpiani, 2007)[11].
Awareness of the warning signs and stages may help avoid damage to the Patellar Tendon. Athletes, coaches, and athletic trainers' knowledge of the five stages of warning signs and risk factors may assist doctors in diagnosing and treating the injury more effectively. The ability to diagnose and treat the injury as early as possible assists doctors in returning patients to physical activities.
References
- De VILLERS, R. et al. (2001). Patellar-Tendon Imaging: Jumper's Knee. Academic Search Premier. EBSCO Host. Karl E. Mundt, Madison, SD. 28 Jan. 2009
- DELANEY, L. (1995). Giving Injuries the Ice. April & May. EBSCO MegaFILE. EBSCO Host. Karl E. Mundt, Madison, SD. 28 Jan. 2009
- DePALMA, M. et al. (2004). Patellar Tendinosis: Acute Patellar Tendon Rupture and Jumper's Knee. Apr. 2004. Academic Search Premier. EBSCO Host. Karl E. Mundt, Madison, SD. 28 Jan. 2009
- DONOHUE (2008). Basketball Season is Here and so is Jumper's Knee. 13 Dec. 2008. Spartanburg Herald Journal. Proquest. Karl E. Mundt, Madison, SD. 26 Jan. 2009
- DRESSENDORFER, R. and ALPER, B. (2007). Patellar Tendinopathy. Apr. 2007. Academic Search Premier. EBSCO Host. Karl E. Mundt, Madison, SD. 28 Jan. 2009
- FERRETTI, M.D. et al. ( 2002). Patellar Tendonosis. Dec. 2002. Academic Search Premier. EBSCO Host. Karl E. Mundt, Madison, SD. 26 Jan. 2009
- KLUCINEC, B. (2001). Recalcitrant Infrapatellar Tendinitis and Surgical Outcome in Collegiate Basketball Player: A Case Report. 2001. Journal of Athletic Training. Proquest. Karl E. Mundt Library, Madison, SD. 26 Jan. 2009
- KONGSGAARD, M. et al. (2007). Region Specific Patellar Tendon Hypertrophy in Humans Following Resistance Training. Oct. 2007. Academic Search Premier. EBSCO Host. Karl E. Mundt, Madison, SD. 26 Jan. 2009
- MATTINGLY, K. (2009). Knee to Know. Aug. and Sept. 2005. EBSCO MegaFILE. EBSCO Host. 28 Jan. 2009
- PEERS, H.E. (2005). Patellar Tendinopathy in Athletes: Current Diagnostic and Therapeutic Recommendations. Academic Search Premier. EBSCO Host. Karl E. Mundt, Madison, SD. 26 Jan. 2009
- VULPIANI, M. et al. (2007). Jumper's Knee Treatment with Extracorporeal Shock Wave Therapy: A Long-term Follow-up Observational Study. 2007. Journal of Sports Medicine and Physical Fitness. Proquest. Karl E. Mundt, Madison, SD. 26 Jan. 2009
Page Reference
If you quote information from this page in your work, then the reference for this page is:
- McDANIEL, L. et al. (2009) Patellar Tendinopathy [WWW] Available from: https://www.brianmac.co.uk/articles/article059.htm [Accessed
About the Authors
Larry W. McDaniel, Ed.D., is an Associate Professor of Exercise Science at Dakota State University, Madison, SD. USA. Dr McDaniel was a First Team All-American football player (USA Football), a Hall of Fame Athlete, and a Hall of Fame Wrestling Coach.
Allen Jackson, M. Ed., is an Assistant Professor of Physical Education and Health at Chadron State College in Chadron, Nebraska (USA). He is well known for his presentations and publications at international conferences focusing on Leadership, Curriculum, and Health.
Laura Gaudet, PhD., is a Professor and Chair of the Department of Counselling, Psychology and Social Work at Chadron State College, Chadron, NE.
Allie Winkle, Dakota State University, is an outstanding student in exercise science.